RECQL4 c.132A>G, p.Glu44=
NM_004260.4:c.132A>G
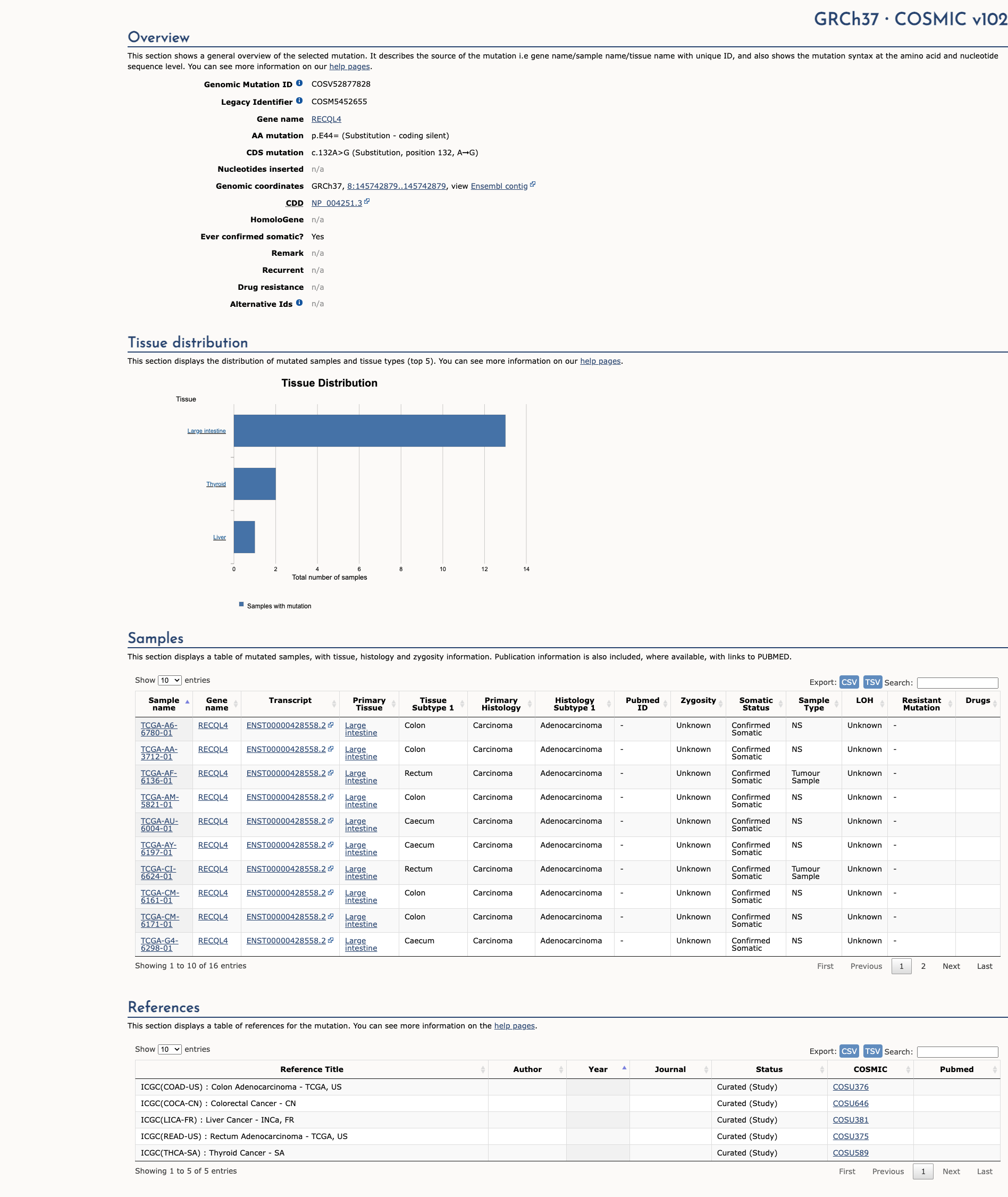
COSMIC ID: COSM5452655
Likely Benign
This synonymous RECQL4 variant is extremely common in the population (MAF=53.7%), has no predicted impact on splicing or function, and is reported as benign in ClinVar. It meets BA1 (Stand Alone) and supporting benign criteria BP4, BP6, and BP7, supporting a classification of Benign.
ACMG/AMP Criteria Applied
BA1
BP4
BP6
BP7
Genetic Information
Gene & Transcript Details
Gene
RECQL4
Transcript
NM_004260.4
MANE Select
Total Exons
21
Strand
Reverse (−)
Reference Sequence
NC_000008.10
Alternative Transcripts
| ID | Status | Details |
|---|---|---|
| NM_004260.3 | RefSeq Select | 21 exons | Reverse |
| NM_004260.2 | Alternative | 21 exons | Reverse |
| NM_004260.1 | Alternative | 21 exons | Reverse |
Variant Details
HGVS Notation
NM_004260.4:c.132A>G
Protein Change
E44=
Location
Exon 3
(Exon 3 of 21)
5'Exon Structure (21 total)3'
Functional Consequence
Loss of Function
Related Variants
Alternate Identifiers
COSM5452655
Variant interpretation based on transcript NM_004260.4
Genome Browser
Loading genome browser...
HGVS InputNM_004260:c.132A>G
Active Tracks
ConservationRefSeqClinVargnomAD
Navigation tips: Use mouse to drag and zoom. Click on features for details.
Clinical Data
Global Frequency
53.7%
Common
Highest in Population
Admixed American
64.5%
Common
Global: 53.7%
Admixed American: 64.5%
0%
0.05%
0.1%
1%
5%
10%+
Allele Information
Total: 240006Alt: 128824Homozygotes: 35121
ACMG Criteria Applied
BA1
This variant is present in gnomAD (MAF= 53.7%, 128824/240006 alleles, homozygotes = 35121) and at a higher frequency in the Admixed American population (MAF= 64.5%, 21369/33126 alleles, homozygotes = 6969). The variant is common (MAF > 1%), supporting BA1 criterion application.
Classification
Benign
Based on 11 submitter reviews in ClinVar
Submitter Breakdown
11 B
Pathogenic
Likely Path.
VUS
Likely Benign
Benign
Publications (0)
No publication details.
Clinical Statement
This variant has been reported in ClinVar as Benign (11 clinical laboratories).
Functional Impact
Functional Domain
Hotspot Status
Not a hotspot
Domain Summary
This variant is not located in a mutational hotspot or critical domain (0 mutations).
Related Variants in This Domain
Computational Analysis
Pathogenicity Predictions
Predictor Consensus
Mixed/VUS
PP3 Applied
No
Additional Predictors
Benign:
CADD: 0.43
VCEP Guidelines
Applied ACMG/AMP Criteria (VCEP Specific)
PVS1
PVS1 (Not Applied) Strength Modified
According to standard ACMG guidelines, PVS1 – Null variant in a gene where loss of function is a known mechanism of disease. The evidence for this variant shows it is a synonymous (E44=) change, not a null variant. Therefore, this criterion is not applied.
PS1
PS1 (Not Applied) Strength Modified
According to standard ACMG guidelines, PS1 – Same amino acid change as a known pathogenic variant but different nucleotide change. The evidence for this variant shows no amino acid change (synonymous). Therefore, this criterion is not applied.
PS2
PS2 (Not Applied) Strength Modified
According to standard ACMG guidelines, PS2 – De novo occurrence confirmed. No de novo data are available for this variant. Therefore, this criterion is not applied.
PS3
PS3 (Not Applied) Strength Modified
According to standard ACMG guidelines, PS3 – Well-established functional studies supportive of a damaging effect. No functional studies exist for this variant. Therefore, this criterion is not applied.
PS4
PS4 (Not Applied) Strength Modified
According to standard ACMG guidelines, PS4 – Increased prevalence in affected versus controls. No case-control data are available. Therefore, this criterion is not applied.
PM1
PM1 (Not Applied) Strength Modified
According to standard ACMG guidelines, PM1 – Located in a mutational hotspot or critical domain without benign variation. This variant is a synonymous change outside known hotspots. Therefore, this criterion is not applied.
PM2
PM2 (Not Applied) Strength Modified
According to standard ACMG guidelines, PM2 – Absent or extremely rare in controls. The evidence shows a high allele frequency (MAF=53.7%) in gnomAD. Therefore, this criterion is not applied.
PM3
PM3 (Not Applied) Strength Modified
According to standard ACMG guidelines, PM3 – Detected in trans with a pathogenic variant for recessive disorders. No trans data are available. Therefore, this criterion is not applied.
PM4
PM4 (Not Applied) Strength Modified
According to standard ACMG guidelines, PM4 – Protein length changes due to in-frame indels or stop-loss. This variant is synonymous with no protein length change. Therefore, this criterion is not applied.
PM5
PM5 (Not Applied) Strength Modified
According to standard ACMG guidelines, PM5 – Novel missense change at an amino acid residue where a different pathogenic missense change has been seen. This variant is synonymous. Therefore, this criterion is not applied.
PM6
PM6 (Not Applied) Strength Modified
According to standard ACMG guidelines, PM6 – Assumed de novo without confirmation. No de novo data are available. Therefore, this criterion is not applied.
PP1
PP1 (Not Applied) Strength Modified
According to standard ACMG guidelines, PP1 – Co-segregation with disease in multiple affected family members. No segregation data are available. Therefore, this criterion is not applied.
PP2
PP2 (Not Applied) Strength Modified
According to standard ACMG guidelines, PP2 – Missense variant in a gene with low benign variation where missense is a common mechanism. This variant is synonymous. Therefore, this criterion is not applied.
PP3
PP3 (Not Applied) Strength Modified
According to standard ACMG guidelines, PP3 – Multiple lines of computational evidence support a deleterious effect. Computational tools (CADD=0.43, SpliceAI=0.01) predict no impact. Therefore, this criterion is not applied.
PP4
PP4 (Not Applied) Strength Modified
According to standard ACMG guidelines, PP4 – Patient phenotype highly specific for a single genetic etiology. No phenotype data available. Therefore, this criterion is not applied.
PP5
PP5 (Not Applied) Strength Modified
According to standard ACMG guidelines, PP5 – Reputable source reports variant as pathogenic without accessible evidence. No such report exists. Therefore, this criterion is not applied.
BA1
BA1 (Stand Alone) Strength Modified
According to standard ACMG guidelines, BA1 – Allele frequency is too high for the disorder. The evidence for this variant shows MAF=53.7% in gnomAD. Therefore, this criterion is applied at Stand Alone strength because the allele frequency far exceeds the threshold.
BS1
BS1 (Not Applied) Strength Modified
According to standard ACMG guidelines, BS1 – Allele frequency greater than expected for the disorder. Although the variant meets frequency criteria, BA1 (Stand Alone) supersedes BS1. Therefore, BS1 is not applied.
BS2
BS2 (Not Applied) Strength Modified
According to standard ACMG guidelines, BS2 – Observed in healthy individuals with full penetrance expected early. No confirmed healthy individual data are available. Therefore, this criterion is not applied.
BS3
BS3 (Not Applied) Strength Modified
According to standard ACMG guidelines, BS3 – Well-established functional studies show no damaging effect. No functional studies exist. Therefore, this criterion is not applied.
BS4
BS4 (Not Applied) Strength Modified
According to standard ACMG guidelines, BS4 – Lack of segregation in affected family members. No segregation data are available. Therefore, this criterion is not applied.
BP1
BP1 (Not Applied) Strength Modified
According to standard ACMG guidelines, BP1 – Missense variant in a gene where only loss of function causes disease. This variant is synonymous. Therefore, this criterion is not applied.
BP2
BP2 (Not Applied) Strength Modified
According to standard ACMG guidelines, BP2 – Observed in trans with a pathogenic variant or in cis. No such data are available. Therefore, this criterion is not applied.
BP3
BP3 (Not Applied) Strength Modified
According to standard ACMG guidelines, BP3 – In-frame indels in repetitive regions without known function. This variant is not an indel. Therefore, this criterion is not applied.
BP4
BP4 (Supporting)
According to standard ACMG guidelines, BP4 – Multiple lines of computational evidence suggest no impact on the gene or gene product. The evidence for this variant shows SpliceAI=0.01 and a low CADD score, indicating no predicted impact. Therefore, BP4 is applied at Supporting strength.
BP5
BP5 (Not Applied) Strength Modified
According to standard ACMG guidelines, BP5 – Variant found in a case with an alternate molecular basis for disease. No case data are available. Therefore, this criterion is not applied.
BP6
BP6 (Supporting)
According to standard ACMG guidelines, BP6 – Reputable source reports variant as benign, but without accessible evidence. The evidence for this variant shows ClinVar classification as Benign by 11 clinical laboratories. Therefore, BP6 is applied at Supporting strength.
BP7
BP7 (Supporting)
According to standard ACMG guidelines, BP7 – Synonymous variant with no predicted impact on splicing. The evidence shows this is a synonymous (E44=) change with SpliceAI=0.01. Therefore, BP7 is applied at Supporting strength.