MLH1 c.1590C>T, p.Phe530=
NM_000249.3:c.1590C>T
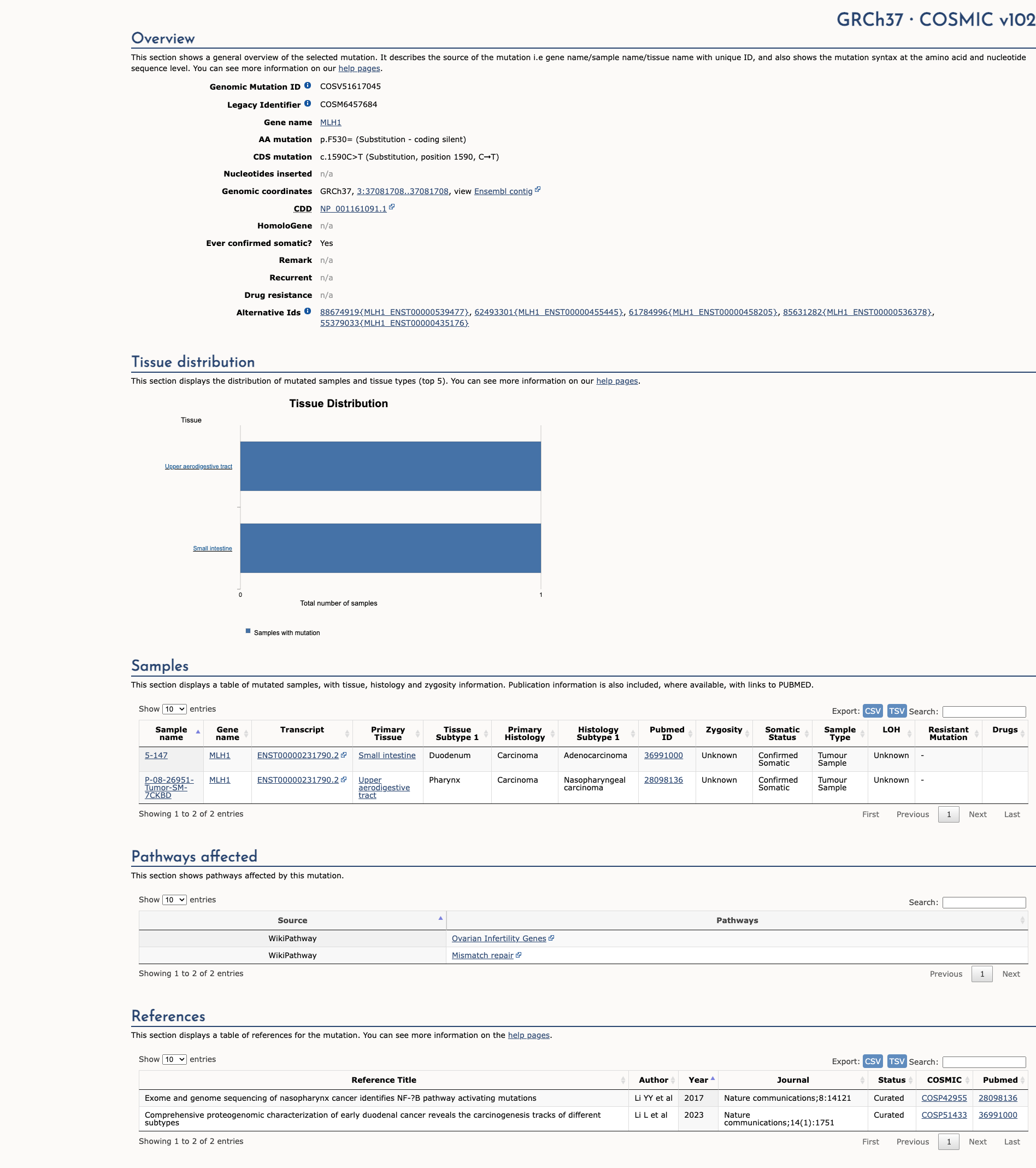
COSMIC ID: COSM6457684
Likely Benign
c.1590C>T (p.F530=) in MLH1 is a synonymous variant with computational and database evidence indicating no impact on splicing or function, and rare population frequency not meeting pathogenic thresholds. Three benign supporting criteria (BP4, BP6, BP7) yield a final classification of Likely Benign.
ACMG/AMP Criteria Applied
BP4
BP6
BP7
Genetic Information
Gene & Transcript Details
Gene
MLH1
Transcript
NM_000249.4
MANE Select
Total Exons
19
Strand
Forward (+)
Reference Sequence
NC_000003.11
Alternative Transcripts
| ID | Status | Details |
|---|---|---|
| NM_000249.3 | RefSeq Select | 19 exons | Forward |
| NM_000249.2 | Alternative | 19 exons | Forward |
Variant Details
HGVS Notation
NM_000249.3:c.1590C>T
Protein Change
F530=
Location
Exon 14
(Exon 14 of 19)
5'Exon Structure (19 total)3'
Functional Consequence
Loss of Function
Related Variants
Alternate Identifiers
COSM6457684
Variant interpretation based on transcript NM_000249.4
Genome Browser
Loading genome browser...
HGVS InputNM_000249:c.1590C>T
Active Tracks
ConservationRefSeqClinVargnomAD
Navigation tips: Use mouse to drag and zoom. Click on features for details.
Clinical Data
Global Frequency
0.00354%
Rare
Highest in Population
European (non-Finnish)
0.00543%
Rare
Global: 0.00354%
European (non-Finnish): 0.00543%
0%
0.05%
0.1%
1%
5%
10%+
Allele Information
Total: 282624Alt: 10Homozygotes: 0
ACMG Criteria Applied
PM2
This variant is present in gnomAD (MAF= 0.00354%, 10/282624 alleles, homozygotes = 0) and at a higher frequency in the European (non-Finnish) population (MAF= 0.00543%, 7/128990 alleles, homozygotes = 0). The variant is rare (MAF < 0.1%), supporting PM2 criterion application.
Classification
Likely Benign
Based on 7 submitter reviews in ClinVar
Submitter Breakdown
5 LB
2 B
Pathogenic
Likely Path.
VUS
Likely Benign
Benign
Publications (0)
No publication details.
Clinical Statement
This variant has been reported in ClinVar as Benign (2 clinical laboratories) and as Likely benign (5 clinical laboratories).
Functional Impact
Functional Domain
Hotspot Status
Not a hotspot
Domain Summary
This variant is not located in a mutational hotspot or critical domain (0 mutations).
Related Variants in This Domain
Computational Analysis
Pathogenicity Predictions
Predictor Consensus
Mixed/VUS
PP3 Applied
No
Additional Predictors
Benign:
CADD: 0.48
VCEP Guidelines
Applied ACMG/AMP Criteria (VCEP Specific) VCEP Guidelines
PVS1
PVS1 (Not Applied) Strength Modified
According to VCEP guidelines for PVS1: 'Very Strong Nonsense/frameshift variant introducing Premature Termination Codon (PTC) at or before codon 753 in MLH1...'. The variant is c.1590C>T, a synonymous change (p.F530=) with no effect on protein coding. Therefore, PVS1 is not applied because the variant does not meet the null variant requirement.
PS1
PS1 (Not Applied) Strength Modified
According to VCEP guidelines for PS1: 'Strong A predicted missense substitution that encodes the same amino acid change with a different underlying nucleotide change previously established by this VCEP as Pathogenic'. The variant is synonymous and does not change amino acid. Therefore, PS1 is not applied.
PS2
PS2 (Not Applied) Strength Modified
According to standard ACMG guidelines for PS2: 'De novo (both maternity and paternity confirmed) in a patient with the disease and no family history'. There are no de novo data provided. Therefore, PS2 is not applied.
PS3
PS3 (Not Applied) Strength Modified
According to VCEP guidelines for PS3: 'Strong Calibrated functional assays with functional odds for Pathogenicity > 18.7'. No functional assays have been performed for this variant. Therefore, PS3 is not applied.
PS4
PS4 (Not Applied) Strength Modified
According to standard ACMG guidelines for PS4: 'The prevalence of the variant in affected individuals is significantly increased compared with controls'. No case-control or case series data are available. Therefore, PS4 is not applied.
PM1
PM1 (Not Applied) Strength Modified
According to standard ACMG guidelines for PM1: 'Located in a mutational hot spot and/or critical functional domain without benign variation'. This is a synonymous variant outside known functional domains. Therefore, PM1 is not applied.
PM2
PM2 (Not Applied) Strength Modified
According to VCEP guidelines for PM2_Supporting: 'Absent/extremely rare (<1 in 50,000 alleles) in gnomAD v4 dataset'. The observed MAF (0.0000354) exceeds the 1/50,000 threshold (0.00002). Therefore, PM2 is not applied.
PM3
PM3 (Not Applied) Strength Modified
According to standard ACMG guidelines for PM3: 'For recessive disorders, detected in trans with a pathogenic variant'. MLH1-associated Lynch syndrome is dominant and no trans data are provided. Therefore, PM3 is not applied.
PM4
PM4 (Not Applied) Strength Modified
According to standard ACMG guidelines for PM4: 'Protein length changes due to in-frame indels or stop-loss variants'. This is a synonymous change. Therefore, PM4 is not applied.
PM5
PM5 (Not Applied) Strength Modified
According to standard ACMG guidelines for PM5: 'Novel missense change at an amino acid residue where a different missense change is pathogenic'. This variant is synonymous. Therefore, PM5 is not applied.
PM6
PM6 (Not Applied) Strength Modified
According to standard ACMG guidelines for PM6: 'Assumed de novo, without confirmation of paternity and maternity'. No de novo data are provided. Therefore, PM6 is not applied.
PP1
PP1 (Not Applied) Strength Modified
According to standard ACMG guidelines for PP1: 'Co-segregation with disease in multiple affected family members'. No segregation data are available. Therefore, PP1 is not applied.
PP2
PP2 (Not Applied) Strength Modified
According to standard ACMG guidelines for PP2: 'Missense variant in a gene with low rate of benign missense variation'. The variant is synonymous. Therefore, PP2 is not applied.
PP3
PP3 (Not Applied) Strength Modified
According to VCEP guidelines for PP3: 'Supporting Predicted splice defect for non-canonical splicing nucleotides using SpliceAI with delta score ≥ 0.2'. SpliceAI predicts no impact (max score 0.09). Therefore, PP3 is not applied.
PP4
PP4 (Not Applied) Strength Modified
According to VCEP guidelines for PP4: 'Strong evidence from tumor MSI-H and/or loss of MMR expression consistent with MLH1'. No tumor or phenotype data are provided. Therefore, PP4 is not applied.
PP5
PP5 (Not Applied) Strength Modified
According to standard ACMG guidelines for PP5: 'Reputable source reports as pathogenic but no evidence available'. The variant is reported as benign in ClinVar, not pathogenic. Therefore, PP5 is not applied.
BA1
BA1 (Not Applied) Strength Modified
According to VCEP guidelines for BA1: 'Stand Alone GnomAD v4 Grpmax filtering allele frequency ≥ 0.001 (0.1%)'. The observed MAF (0.0000354) is below 0.001. Therefore, BA1 is not applied.
BS1
BS1 (Not Applied) Strength Modified
According to VCEP guidelines for BS1: 'GnomAD v4 Grpmax filtering allele frequency ≥ 0.0001 and < 0.001'. The observed MAF (0.0000354) is below 0.0001. Therefore, BS1 is not applied.
BS2
BS2 (Not Applied) Strength Modified
According to VCEP guidelines for BS2: 'Observed in trans with a pathogenic variant in Lynch syndrome cancer patients without CMMRD'. No co-occurrence data available. Therefore, BS2 is not applied.
BS3
BS3 (Not Applied) Strength Modified
According to standard ACMG guidelines for BS3: 'Well-established functional studies show no damaging effect on gene or gene product'. No functional assay data are available. Therefore, BS3 is not applied.
BS4
BS4 (Not Applied) Strength Modified
According to standard ACMG guidelines for BS4: 'Lack of segregation in affected members of a family'. No segregation data are available. Therefore, BS4 is not applied.
BP1
BP1 (Not Applied) Strength Modified
According to standard ACMG guidelines for BP1: 'Missense variant in a gene for which primarily truncating variants cause disease'. The variant is synonymous. Therefore, BP1 is not applied.
BP2
BP2 (Not Applied) Strength Modified
According to standard ACMG guidelines for BP2: 'Observed in trans with a pathogenic variant for a dominant disorder'. No such data are available. Therefore, BP2 is not applied.
BP3
BP3 (Not Applied) Strength Modified
According to standard ACMG guidelines for BP3: 'In-frame deletions/insertions in a repetitive region without a known function'. The variant is synonymous. Therefore, BP3 is not applied.
BP4
BP4 (Supporting)
According to VCEP guidelines for BP4: 'Supporting For intronic and synonymous variants: SpliceAI predicts no splicing impact with delta score ≤ 0.1'. SpliceAI predicts max delta score 0.09. Therefore, BP4 is applied at Supporting strength because computational evidence shows no impact on splicing.
BP5
BP5 (Not Applied) Strength Modified
According to VCEP guidelines for BP5: 'Tumor data inconsistent with gene-disease mechanism'. No tumor or clinical case data are provided. Therefore, BP5 is not applied.
BP6
BP6 (Supporting)
According to standard ACMG guidelines for BP6: 'Reputable source recently reports variant as benign but the evidence is not available'. ClinVar lists this variant as Benign or Likely Benign by multiple labs. Therefore, BP6 is applied at Supporting strength because a reputable source reports a benign classification.
BP7
BP7 (Supporting)
According to VCEP guidelines for BP7: 'Supporting A synonymous (silent) variant at or beyond -21/+7 exonic; may satisfy BP7 if no splicing impact'. This is a synonymous change outside splice consensus and SpliceAI delta score ≤ 0.1. Therefore, BP7 is applied at Supporting strength.